Endodontic Diagnosis
26 Endodontic Diagnosis
Pratik Kamalkant Shah and Bun San Chong
Summary
The diagnosis of pulpal and periradicular diseases, based on clinical observations and associated tests, can be challenging. The application of interview skills, clinical experience, scientific knowledge, and intuition is essential for accurate diagnosis. Appropriate treatment must only be planned and provided after a diagnosis is reached.
In this chapter, a systematic diagnostic process involving detailed history taking and thorough clinical and radiographic examination is described. The value and limitations of routine and special tests, including sensitivity and specificity of pulp tests, are reviewed. The diagnosis and management of a cracked tooth can be challenging, so techniques to help are highlighted. There is discussion on the benefits and limitations of radiographic examinations using two- and three-dimensional radiography, including relevant guidelines. The section on referred pain summarises potential nonodontogenic causes.
The limitations of pulpal and periradicular diseases classification systems are considered. Based on the information gained from the diagnostic process, remedial treatment can be planned and provided; nowadays, this may include treatment modalities directed towards preservation of the vital pulp.
26.1 Introduction
Diagnosis can be defined as ‘the process of determining the nature of a disease or disorder and distinguishing it from other possible conditions’ [1]. Hence, the diagnostic process involves the application of scientific knowledge and clinical experience in the systematic evaluation of a patient’s complaint to confirm the exact cause of a disease or problem. Errors or deficiencies can lead to misdiagnosis and, consequently, incorrect management including unnecessary or inappropriate interventions and unfavourable outcomes.
In Endodontics, the purpose of diagnosis is to determine the pulpal and periradicular status and presence of associated disease based on clinical observations and tests so that the cases can be appropriately managed. The anatomically confined nature of pulp and periradicular tissues makes direct observation, sampling, or testing to determine their health status difficult to perform. Therefore, a diagnostic process comprising assessments of the patient history, clinical signs and symptoms, and radiological information is required for inferred verification of their health status.
The American Association of Endodontists has produced an endodontic competency document that details the standards expected from dentists for the diagnosis of endodontic problems [2]. To ensure an accurate diagnosis, a dentist must thoroughly interview the patient to help scrutinise the subjective data and objectively explore all relevant clinical and radiographic information [2, 3]. A sound interpretation of this information, based on knowledge of disease processes involved, presenting features and classification, should help judge the correct diagnosis and execute remedial treatment on an urgent or emergency basis [2]. These essential clinical skills are summarised in Figure 26.1. Additionally, dentists must also be able to assess, diagnose, and provide emergency care or refer patients presenting with acute dental trauma [2].

Figure 26.1 Illustrative roles of a dentist in the diagnosis and treatment of a patient’s endodontic complaint.
Unfortunately, patients may occasionally present with signs and symptoms that are not consistent with observations made during clinical examination. In these cases, careful interpretation of the diagnostic information gleaned, clinical experience, and informed intuition are imperative in the quest to identify the reason/s for the presenting complaint. This chapter discusses the stages of the diagnostic process including the relevance and limitations of clinical tests.
Key Points
- The role of the clinician in the diagnostic process
- The importance of clinical experience and intuition in diagnosing challenging cases
- Adopting a systematic approach for history taking, examination, and analysis of diagnostic information gathered
26.2 History Taking
History taking is the first step of the diagnostic process in which a comprehensive interview of the patient is undertaken concerning the presenting problem and any relevant dental, medical, or social factors. During this interview, the clinician should always ask open-ended questions to better gather crucial and subtle details that may help in the diagnostic process. Clinical records should reflect all pertinent and accurate descriptions of the patient’s complaint.
26.2.1 Presenting Problem
The presenting complaint should be recorded in the patient’s own words as much as possible; however, for children and those with special needs or impaired capacity, the description reported by the responsible adult, carer, or relative should be recorded.
Pain is usually a common complaint. A thorough and structured history of the patient’s pain complaint can be obtained by following the mnemonic, SOCRATES (Table 26.1). It is important to remember that patients may be vague or inaccurate when describing pain, given its subjective nature.
Table 26.1 History of pain complaint – key questions to ask the patient.
| Features | Example of questions |
|---|---|
| Site | Where is the pain located? |
| Onset | When did the pain start? Is the pain sudden or gradual? Is the pain progressive or regressive? |
| Character | How would you describe the pain – sharp/stabbing, dull/throbbing, or other characteristics? |
| Radiation | Where and how far does the pain spread? |
| Associations | Any other signs and symptoms, for example, worse when supine, fever, swelling, sinus tract, taste, sensory disturbance? |
| Time course | How long does the pain last – seconds, minutes, or hours? Is the pain spontaneous, intermittent, or continuous? |
| Exacerbating/relieving factors | Do hot/cold foods and/or drinks worsen the pain? Does chewing or biting worsen the pain? To what extent do painkiller medication relieve the pain? |
| Severity | How would you rate the pain severity from 1–10 (10 being the maximum severity)? Has the pain woken you up from sleep? |
Clinicians should be aware that pulps can become necrotic without causing any pain (painless pulpitis) [4–6]. Patients may only be prompted to seek advice or treatment following other developments; for example, cusp fracture, discolouration, or development of a sinus tract associated with the necrotic pulp.
26.2.2 Dental History
Obtaining a thorough dental history of the patient will further aid in the exploration of the presenting complaint. Details of previous restorative or endodontic interventions, parafunctional habits, and patient compliance may help the clinician understand the cause of the problem and contribute towards determining management and prognosis of any interventions. This is particularly relevant, for example, in dental resorption cases as a history of previous dental trauma, orthodontic treatment, periodontal treatment or disease, tooth lightening, and restorative or surgical procedures may help to identify cause(s) of the complaint [7, 8].
26.2.3 Medical History
A detailed medical history should be obtained as it may help in the diagnosis and management of the patient’s complaint and impact on treatment outcome. Certain systemic diseases (Table 26.2) that have extra- or intraoral manifestations may have relevance to the presentation of the patient’s complaint.
Table 26.2 Extra- and intraoral manifestations of systemic diseases.
| Clinical/radiographic presentation | Systemic disease |
|---|---|
| Lymph node enlargement | Lymphomas |
| Paraesthesia of oral tissues | Iron deficiency anaemia, pernicious anaemia, leukaemia |
| Dental root resorption (multiple sites) | Paget’s disease, hyperparathyroidism, chronic kidney disease, liver disease |
| Teeth sensitivity, xerostomia | Radiation therapy |
| Teeth mobility | Multiple myeloma |
| Dental abscesses | Diabetes mellitus, immunocompromised patients |
| Dental pain (referred) | Trigeminal neuralgia, ischaemic heart disease, multiple sclerosis, acute sinusitis, fibromyalgia, migraines, cluster headaches |
| Bone pain/loss of trabeculae | Sickle cell anaemia |
Medical contraindications to root canal treatment, including recent myocardial infarction, uncontrolled hypertension, and uncontrolled diabetes, must also be considered [2]. For such cases, treatment may need to be appropriately delayed or referred to a specialist.
26.2.4 Antibiotic Cover
It is important to follow applicable guidelines on the use of antibiotic prophylaxis. A position statement by the European Society of Endodontology [9] on the use of antibiotics in endodontics recommends prophylactic use for patients undergoing nonsurgical/surgical root canal treatment who are immunocompromised (dependent on a risk-benefit analysis), at high risk of developing infective endocarditis, have prosthetic joints fitted within the preceding 3 months, or are exposed to high-dose radiation in head and neck, and also for patients requiring surgical endodontics receiving intravenous bisphosphonates [9, 10]. Where there is a lack of clarity on the need for antibiotic prophylaxis, the patient’s medical care team should be consulted.
26.2.5 Social History
Important details from the social history including smoking, alcohol consumption, recreational drug use, occupation and family or work circumstances may help identify psychosocial factors that may be associated with dental and medical problems; it also provides clues as to the patient motivation or attitude towards treatment [11]. Gathering the history of the presenting complaint and the dental, medical, and social histories will facilitate the clinician and allow the arrival of a tentative diagnosis.
Key Points
- A thorough history taking relies on good patient interview skills
- The mnemonic, SOCRATES, may be used to comprehensively cover the pain history
- Awareness of extra- and intraoral manifestations of systemic diseases is essential
26.3 Clinical Examination
The clinical examination involves a comprehensive extra- and intraoral assessment of the patient, with a focus on the concerned tooth or teeth and soft tissues, and supported by relevant radiographic investigations.
26.3.1 Extraoral assessment
The extraoral examination includes visual observation of any facial asymmetry that may denote the presence of a swelling, changes in skin colouration (redness or bruising), followed by palpation of cervical and submandibular lymph nodes, temporomandibular joints (TMJs), facial bones, and muscles of mastication. Any swelling present should be categorised as localised or diffused, firm or fluctuant, and with or without an extraoral sinus tract. The spread of infection into the soft tissue spaces is determined by the relative position of the diseased tooth apex to the adjacent level of muscle insertion on the maxilla or mandible. Therefore, extraoral swellings of endodontic origin often involve the canine, buccal, and submandibular spaces (Figure 26.2). Tenderness of muscles of mastication is often related to parafunctional habits and has a role in the development of myofascial pain; this may be a contributory factor to the patient’s presenting complaint.

Figure 26.2 Extraoral swelling on the left side of the face involving the buccal and infratemporal spaces.
26.3.2 Intraoral assessment
An initial part of the intraoral examination is an assessment of the extent of mouth opening; if limited, this may impede access when carrying out treatment. If a patient has a sensitive gag reflex, this should also be noted because this may also impact on treatment.
A thorough visual assessment and palpation of the soft tissues, including the salivary glands, tongue, floor of the mouth, palate, vestibules, and cheeks, is performed under adequate illumination and/or magnification. Pertinent details of any ulceration, swellings, sinus tracts, colour changes, altered sensation, or soft tissue injuries should be noted. Intraoral swellings (Figure 26.3) can occur in the sublingual or buccal spaces and should, just like extraoral swellings, be characterised accordingly. Swellings or haematomas affecting the floor of the mouth may pose a threat to the airway and should be kept in mind. Intraoral sinus tracts should be traced with a gutta-percha point to help identify its source (Figure 26.4). Any abnormal changes in sensation should be mapped, recorded, and compared with the contralateral side.

Figure 26.3 A fluctuant intraoral swelling adjacent to a maxillary right first premolar.
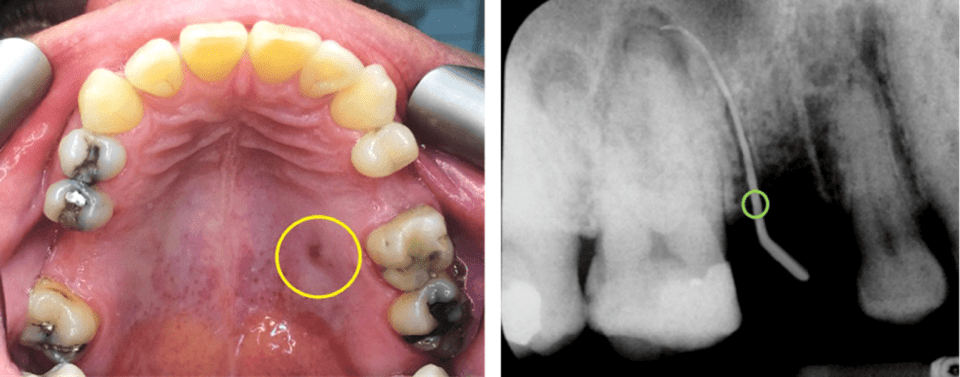
Figure 26.4 Maxillary left first molar: (left) an intraoral palatal sinus (yellow circle); (right) the sinus tract opening (green circle) traced with a gutta-percha pointed to this tooth.
Assessment of the oral hygiene, periodontal health, caries incidence, restorative state of the dentition, tooth surface loss and occlusion should also be performed. The presence of occlusal interferences may, for example, mimic symptomatic apical periodontitis.
The tooth or teeth in question must be assessed further. The presence of cracks, large restorations, wear facets, or discolouration may help to identify the reason/s for the patient’s complaint. Tooth discolouration may indicate that pulpal health is compromised as a result of dental trauma (reddish-purple or greyish); other examples include pulp canal obliteration (yellowish), pulp necrosis (greyish or brownish-grey), or dental resorption (pink spot for external cervical resorption or internal inflammatory resorption) (Figure 26.5).

Figure 26.5 Tooth discolouration (from left to right): yellowish maxillary left central incisor due to pulp canal obliteration, greyish maxillary left lateral incisor due to pulp necrosis, and pink cervical spot on the distobuccal aspect of the mandibular left canine with external cervical resorption (circled).
Routine tests of the tooth/teeth concerned involve palpation of the overlying mucosa, tooth percussion, mobility, and periodontal assessment. Special tests, such as thermal and electric pulp testing, are carried out to provide an indication of pulpal health status; adjacent teeth may be used as controls for comparison purposes.
Following history taking, extra- and intraoral examination, and relevant special tests, a differential or provisional diagnosis may be possible. Radiographic images of the tooth or teeth of interest are taken to help provide more diagnostic information, helping to narrow the differential diagnosis. Often, multiple radiographic images at different planes may be required to judge the location, extent, and involvement of the disease process [12]. Occasionally, three-dimensional imaging techniques, such as cone-beam computer tomography (CBCT), may be indicated to provide more diagnostic information; see Section 26.3.4.
Routine assessments, special tests, and radiographic images are subject to interpretation inaccuracies. It is crucial that clinicians understand the value, relevance, and limitations of the results from these tests and radiographic images. Testing of a contralateral tooth must always be performed to act as a control for routine and special tests. In the absence of a contralateral tooth, a similarly sized tooth on the opposite side of the arch or an ipsilateral tooth may be selected.
26.3.3 Routine Tests
Palpation, by applying digital pressure on the overlying mucosal surface of the tooth, is used to assess for the presence of inflammation of the periodontium (Figure 26.6). Palpation of soft tissue swellings also help to identify important characteristics, whether it is fluctuant or firm, and localised or diffused. For muscles of mastication (e.g. lateral pterygoid), palpation may be useful in identifying suspected cases of parafunctional activity.

Figure 26.6 Palpation testing of the buccal mucosa overlying the apex of the maxillary right central incisor.
Percussion, generally performed axially, with a gloved finger or the blunt end of a dental instrument and with a force of 2–4 N, is used to assess apical periodontal ligament inflammation (Figure 26.7) [13, 14]. Occasionally, inflammation of the periodontal ligament may occur on the lateral root surface; thus, nonaxial (lateral) tapping of the tooth should also be performed (Figure 26.7).

Figure 26.7 Percussion testing of the maxillary right lateral incisor using a mirror handle being performed axially (left) and laterally (right).
From an endodontic perspective, percussion tests are only useful when the disease process has involved the periodontal ligament and when mechano-receptors on Aβ fibres are activated in response to tissue fluid pressure changes. Thus, the percussion test is useful for detecting symptomatic apical periodontitis, vertical root fractures, and sometimes, root perforations. However, teeth may also be tender to percussion in cases with severe periodontal disease, endodontic-periodontal lesions, traumatic occlusion, parafunctional activity, and following dental trauma. Additionally, in trauma cases, a high-pitched or metallic quality of sound produced during percussion testing may indicate presence of ankylosis/external replacement resorption [7], or lateral luxation with concomitant alveolar process fracture [15].
Tooth mobility evaluation provides an indication of the level of periodontal support. The ends of two mirror handles may be used to check for tooth mobility in the buccolingual or buccopalatal direction. Tooth mobility is graded using Miller’s classification [16]:
Class 1: <1 mm horizontal movement
Class 2: >1 mm horizontal movement
Class 3: >1 mm horizontal and vertical movement
In cases of dental trauma, an absence of abnormal mobility may suggest that a tooth is ankylosed [7]; it may also indicate lateral luxation with concomitant alveolar process fracture [15].
Various specialised devices, such as periodontometers, the electromagnetically driven periotest, and Konermann’s novel intraoral measuring device have been developed to help quantify the degree of tooth mobility; however, these devices are cumbersome, technique sensitive, and/or time consuming to utilise [17].
A periodontal assessment is carried out using a periodontal probe to ascertain the health of the periodontium and help in the detection of endodontic-periodontal lesions and periodontal abscesses. A basic periodontal examination (BPE) and further assessment, including a six-point pocket chart and relevant radiographs, are also necessary to evaluate periodontal health. V-shaped probing profiles with/without bleeding, generalised/localised gingival recession, and horizontal and furcal bone loss indicate the presence of periodontitis. Staging and grading of periodontitis, based on clinical findings and radiographs, will help inform clinicians on the severity, extent, and complexity of the disease, treatment options, and long-term prognosis [18].
Endodontic-periodontal lesions, without root damage, are classified as occurring in either periodontitis or nonperiodontitis patients, with further categorisation depending on the probing profile and the number of tooth surfaces involved [18, 19]. Accordingly, Grade 1 represents a narrow deep pocket on one tooth surface, Grade 2 signifies a wide deep pocket on one tooth surface, and Grade 3 denotes deep pockets on more than one tooth surface [18, 19].
In cases with severe periodontal disease, involvement of the root apex or a lateral canal may result in pulp necrosis and the development of a deep and wide V-shaped probing profile, as observed in Grade 2 and Grade 3 endodontic-periodontal lesions [19, 20] (Figure 26.8). Due to the advanced periodontitis, with furcation involvement and severe bone loss, endodontic-periodontal lesions in periodontitis patients will generally have a hopeless or poor long-term prognosis.

Figure 26.8 Grade 3 endodontic-periodontal lesions affecting the maxillary left second premolar and first molar in a patient with chronic periodontitis.
A deep, narrow probing profile in the absence of periodontitis may indicate the presence of a sinus tract, opening at the gingival margin; it may also be due to root damage following vertical root fracture, or iatrogenic or pathological root perforations [19, 20]. Concomitant periodontal inflammation may result a narrow probing depth widening to become more V-shaped [21] (Figure 26.9). Such endodontic-periodontal lesion, without root damage, in a nonperiodontitis patient has a favourable prognosis following combined periodontal and endodontic treatments.

Figure 26.9 Grade 2 endodontic-periodontal lesion affecting the mandibular left second molar in a nonperiodontitis patient.
Deep, narrow probing depths with bleeding on probing in the presence of positive pulp sensitivity tests may indicate the presence of developmental grooves or enamel spurs (pearls). In cases where a developmental groove is deep, pulp necrosis can occur yielding negative pulp sensitivity test results, and a periodontal abscess may develop. Furcation defects with or without gingival swellings may indicate the presence of pulp floor perforations; it may also be due to coronal pulp necrosis leading to periodontal inflammation through patent furcal accessory canals [19]. Subgingival cervical dentinal defect associated with external cervical root resorption may be detected during periodontal probing; there is usually heavy bleeding associated with inflammation of the overlying granulation tissue [7, 22, 23] (Figure 26.10).

Figure 26.10 Cervical defect (circled) associated with external cervical root resorption on the mandibular left first premolar.
26.3.4 Special Tests
Commonly, special tests performed include thermal and electric pulp tests for indirect assessment of pulpal health status. Other tests include test cavity preparation, selective analgesia, transillumination, staining, and the bite test. These tests can be grouped and categorised based on their respective objectives as shown in Table 26.3. Newer and experimental testing methods have been described in the literature, for example, Laser Doppler Flowmetry (LDF), pulp oximetry, and biological inflammatory markers.
Table 26.3 Classification of clinical testing methods based on objectives.
| Test | Category and objective | Method |
|---|---|---|
| Routine | Periradicular tests To evaluate periodontal health status | Palpation |
| Percussion | ||
| Mobility assessment | ||
| Periodontal assessment | ||
| Special | Pulp sensitivity tests To indirectly evaluate pulpal health status via nerve innervation | Thermal test |
| Electric pulp test | ||
| Test cavity | ||
| Air desiccation | ||
| Dentinal probing | ||
Pulp vitality tests To directly evaluate pulpal health status via blood flow detection | Laser Doppler Flowmetry | |
| Pulp oximetry | ||
| Crack detection techniques: To evaluate the presence of cracks or root fractures | Bite test | |
| Staining | ||
| Transillumination | ||
| Surgical exposure | ||
| Others | Selective analgesia | |
| Biological inflammatory markers | ||
26.3.4.1 Terminology: Sensitivity, Sensibility, and Vitality
‘Sensitivity’, ‘sensibility’, and ‘vitality’, in relation to special tests to ascertain pulpal health status, are often used interchangeably. A subject for debate, depending on preference, the terminology may lead to confusion. It is impossible to discourse at length this subject. In this chapter, ‘vitality’ refers to the presence of pulpal blood flow, whereas a test for ‘sensitivity’ is to help ascertain if a tooth reacts or is responsive to an applied stimulus, whereas ‘sensibility’ refers to multimodal sensory perception, for example simultaneous perception of temperature and pressure.
26.3.4.2 Pulp Sensitivity Tests
These tests provide an indication of the pulpal health status indirectly by assessing the innervation of the coronal pulp tissue (Aδ and C fibres) [3]. Myelinated Aδ fibres innervating the periphery of the pulp chamber have low excitation thresholds and activation by dentinal fluid movement (hydrodynamic activation [24]) produces a short, well-localised, and sharp pain [25, 26], whereas unmyelinated C fibres are more centrally located in the pulp, have higher excitation thresholds, and when activated following intense pulp tissue damage produce a dull, poorly localised pain that may radiate [27–29]. When inflammation first develops in the pulp, the Aδ fibres are the first to be excited. Sensitivity to cold is common, but as the inflammation spreads and pulp tissue deteriorates, C fibres become involved and sensitivity to heat is more common. Therefore, the aim of pulp sensitivity testing is to elicit a hydrodynamic, or a tissue injury, response via the pulp’s nerve supply [30]. Thus, knowledge of the development, structure, and function of the pulpal neurovascular supply, including the plexus of Raschkow, is central to the interpretation of the test results and their limitations.
Thermal tests involve the momentary application of cold or heat stimuli to the incisal or middle third of the buccal/labial surface of the tooth’s crown to reproduce symptoms [30–32]. Therefore, the selection of a cold or heat test depends on the patient’s presenting complaint. In the absence of thermal symptoms, the cold test is used to assess pulp sensitivity because it is considered more reliable and easier to use.
Cold tests can be carried out using ice sticks, ethyl chloride (-4oC), tetrafluoroethane (-26.2oC), propane-butane mixture (-50oC) (Figure 26.11), or carbon dioxide snow (-78oC). Chemicals with low melting points, such as propane-butane mixture or carbon dioxide snow, when used for pulp sensitivity testing result in strong hydrodynamic responses [29, 32], which makes them suitable for testing teeth with thick enamel or tertiary dentine layer, full-coverage coronal restorations, and immature roots [30, 33, 34]. To avoid thermal damage to pulp tissue, tooth contact with such chemicals should not exceed 5 seconds; however, longer contact time or repeated testing may be necessary for crowned teeth or teeth with large restorations. It must be noted that the results of the cold test can be highly subjective and, as discussed later, dependent on various patient and tooth factors [35].

Figure 26.11 A propane-butane mixture spray (Endo-frost, Roeko, Langenau, Germany) applied on a cotton wool pellet being used for pulp sensitivity testing of the maxillary right lateral incisor.
For healthy or non-irreversibly inflamed pulps, cold tests activate Aδ fibres hydrodynamically following the contraction and outward flow of dentinal fluid and result in a brief, sharp pain that disappears when the stimulus is removed [24, 36]. In inflamed pulps, an exaggerated response to stimulation (hyperalgesia) followed by a dull lingering pain, or a delayed intensification of pain after stimulation (C fibre activation), suggests that the pulp is irreversibly inflamed, whereas a negative response may imply that the pulp is necrotic. In some cases of irreversible pulpitis or pulp necrosis, allodynia develops as C fibres in the diseased pulp is stimulated by the normal body temperature, and the application of cold may actually provide temporary pain relief. Cold test is useful in monitoring the pulp status of immature and young mature teeth, or differentiating related pathological entities; for example, internal inflammatory resorption with perforation (negative response) from external cervical resorption (positive response).
Heat tests may be performed using warm gutta-percha, thermo-electric heat sources, heated dental instruments, frictional heat generated from a prophylactic cup, or the application of warm water (Figure 26.12). When using warm gutta-percha, contact with the tooth should not exceed 5 seconds due to the risk of damaging healthy pulp tissue [37]. The results of heat tests may be variable given the temperature of the stimulus, the temperature differential, and the rate of heat transfer through the tooth [32]; thus, the test results should be interpreted with caution.

Figure 26.12 Demonstrating the use of warm gutta-percha for the heat test.
Unlike cold tests, the hydrodynamic activation of Aδ fibres in healthy or inflamed pulp may be slow. Short-lasting sharp pain is initially produced, which on continued stimulation results in a dull radiating pain followed by an increase of pulp tissue pressure and C fibre activation. For necrotic pulps, there is generally no response. Thus, heat test can only ascertain necrotic pulps from inflamed/heathy pulps [3]; it cannot differentiate between reversible or irreversible pulpal inflammation.
Bathing individual teeth with warm or cold water following dental dam isolation can be performed to help determine pulp sensitivity status for teeth that are crowned or have large restorations. In teeth with vital pulps, a hydrodynamic response is elicited due to the temperature difference, whereas teeth with nonvital pulps will not produce any response.
Electric pulp testing (EPT) is performed using a device in which a gradually increasing current applied to the tooth via an electrode in contact with the cuspal/incisal tip (Figure 26.13). For healthy or inflamed pulps, Aδ fibres are stimulated at low current levels, where hydrodynamic activation occurs through ionic shift in dentinal fluid, resulting in a short sharp or tingling sensation [38]; at higher current levels, C fibres become involved evoking a dull lingering pain. For necrotic pulps, there is no such response [39]. EPT readings should not be used to quantify the level of pulpal inflammation; it only provides an indication of loss of pulpal vitality, e.g. pulp necrosis or pulpless teeth [4, 40, 41].

Figure 26.13 Demonstrating the use of an EPT device (Digitest 3TM, Parkell, Edgewood, NY, USA) and position of the conducting medium-coated electrode on an isolated maxillary right lateral incisor.
Due to the ionisation effect on dentinal fluid, EPT is particularly useful in establishing the health status of teeth that had affected by pulp canal obliteration, or where thermal tests are inconclusive [42]. EPT is technique-sensitive and correct position of the electrode over the cuspal or incisal tips, adequate tooth isolation, and use of a conducting medium are necessary [43]. Testing of teeth with full coverage crowns and large metallic restorations may be difficult unless there is an exposed root surface to allow the application of the electrode. A control tooth, ideally contralaterally, should be chosen and tested to provide a reference measurement.
Clinicians may be concerned about the use of dental ultrasonic and electronic devices during examinations and treatment for patients with implanted medical electronic devices. An in vivo study [44] found no effect on the function of the pacemakers with the use of EPT devices, electronic apex locators, and ultrasonic equipment. However, due to a paucity of similar studies, the use of EPT devices should be treated with caution or avoided in patients with pacemakers, implantable cardioverter defibrillators, or cochlear ear implants [2]. An in vitro study [45] found that EPT devices had a greater risk of causing interference than electronic apex locators and ultrasonic equipment.
Test cavities, probing, or desiccation (air-drying) of exposed dentine may also activate Aδ fibres, and in healthy pulps, it is characterised by short, sharp pain indicating normal dentine sensitivity. Cases with dentine hypersensitivity exhibit a heightened sharp response that subsides rapidly. However, the absence of a response does not necessarily indicate a nonvital pulp. Test cavities are now considered an archaic and destructive form of evaluation and should only be limited to exceptional cases where other testing modalities are impossible.
26.3.4.2.1 Limitations of Pulp Sensitivity Tests
It is important to bear in mind that the patient’s response to these tests are subjective and may be influenced by patient factors, for example, anxiety [46–48]. False negative or positive results are possible. The thickness of the enamel and dentine, presence of large direct/indirect restorations, concentration of nerve fibres in the adjacent pulp tissue, and orientation of dentinal tubules may all affect the results of pulp sensitivity tests. Since the concentration of nerve fibres is the greater, and the orientation of dentinal tubules is favourable at the cusp or incisal tips, thermal tests and EPT are more likely to elicit a response [49–51]. Unfortunately, with these tests, the health of the radicular pulp tissue is unknown because only the coronal pulp is being tested. Thus, with the exception of EPT and necrotic pulps, there is not necessarily any accurate correlation between the histopathological status of the pulp and the responses to pulp sensitivity testing [4]. Furthermore, the status of pulpal innervation does not necessarily correspond with the presence or absence of a vascular supply [52, 53]. This limits the use of certain pulp sensitivity tests resulting in false positives and negatives; for example:
- EPT or thermal tests for multi-rooted teeth, where the disease processes have affected at least one root. Pulp sensitivity tests may produce conflicting or inconsistent results due to defensive compartmentalisation [54] and maintenance of pulp vitality through unaffected roots.
- EPT and cold test for partially necrotic canals, where Aδ fibres continue to remain active.
- Necrotic teeth with suppuration within root canals that erroneously respond to EPT [41].
- EPT and thermal tests for teeth that have undergone full pulpotomies, where no responses may occur, yet the radicular pulp may still be vital.
- EPT and thermal tests in teeth that have had regenerative endodontic procedures.
- Thermal testing for teeth with tertiary dentine deposition, or pulp canal obliteration, where there is little or no hydrodynamic fluid movement. Thermal testing for such teeth is usually inconclusive [55]; however, EPT is more reliable, often producing an immediate response [4].
- EPT for immature and young mature teeth, where the plexus of Raschkow may not be fully developed [3, 30, 33]. As EPT is more reliable in detecting necrotic pulps of mature teeth [4], cold tests with large temperature differentials are better for such teeth [33].
- EPT or thermal tests for teeth that have suffered recent (0–3 months) dental trauma, where the repair of pulpal neural supply is preceded by the revascularisation and proliferation of pulp tissue [56, 57]. Negative responses during this period suggest pulp is damaged, and diagnosis of pulp necrosis must be made in conjunction with the presence of two or more corroborating clinical signs and symptoms. Pulp sensitivity testing can, however, be used to monitor recovery of the damaged pulp [15].
- Teeth undergoing orthodontic tooth movement, where transitory inflammation of the pulp increases the threshold for EPT [58].
Table 26.4 highlights various false positives and negatives specific to each pulp sensitivity test. It is important for a discerning clinician to be aware of these limitations in order to avoid misdiagnosis.
Table 26.4 False positives and negatives of pulp sensitivity tests.

0 Comments